Treating a large abscess depends on its size, location, severity, and underlying cause. However, in general, here’s how a large abscess is managed:
🚨 Medical Warning
If you suspect a large or deep abscess, especially with signs of fever, spreading redness, or systemic illness, you should seek medical attention immediately. Attempting to drain a large abscess at home can be dangerous and lead to severe infections or complications.
✅ Standard Medical Management of a Large Abscess
1. Assessment by a Healthcare Provider
-
Physical exam
-
Ultrasound or imaging (for deep abscesses like in the abdomen, breast, or perirectal area)
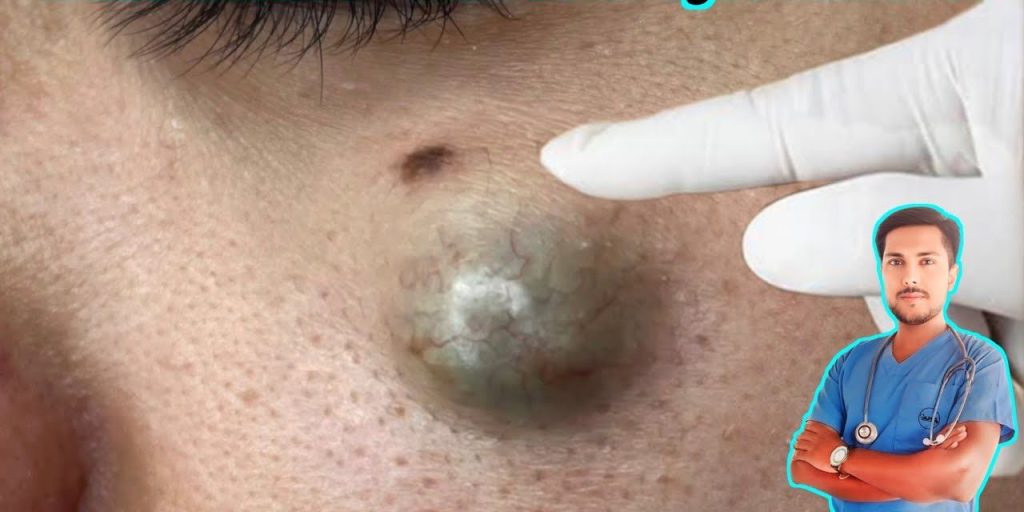
2. Incision and Drainage (I&D)
This is the primary treatment for most large abscesses.
-
Local or general anesthesia (depending on location)
-
Sterile incision over the abscess
-
Drainage of pus
-
Irrigation with saline
-
Packing with gauze if deep, to keep the cavity open and allow continued drainage
3. Antibiotics
Not always necessary for small abscesses but usually given for large abscesses, especially if:
-
The patient has fever
-
The infection has spread (cellulitis)
-
There are comorbidities (e.g., diabetes)
-
The abscess is in a high-risk area (e.g., face, groin)
Common antibiotics include:
-
Clindamycin
-
Trimethoprim-sulfamethoxazole (Bactrim)
-
Amoxicillin-clavulanate
-
Doxycycline
4. Follow-up and Wound Care
-
Daily dressing changes if packed
-
Monitoring for reaccumulation or signs of worsening infection
-
Repeat drainage if it refills
❌ Do NOT:
-
Attempt to squeeze or pop a large abscess
-
Use a needle or knife to drain it at home
-
Ignore signs of spreading infection (red streaks, fever, chills)
🩺 Medical Management of Large Abscesses
1. Assessment and Diagnosis
A thorough evaluation is essential to determine the appropriate treatment for a large abscess. This includes:
-
Clinical Examination: Identifying signs such as redness, swelling, warmth, and fluctuance.
-
Imaging: For deep or non-visible abscesses, ultrasound or CT scans may be employed to assess size, location, and the presence of loculations .
2. Incision and Drainage (I&D) Procedure
I&D is the gold standard for treating large abscesses. The procedure involves:
-
Anesthesia: Administering local anesthesia (e.g., 1% lidocaine) to the affected area.
-
Incision: Making a linear or elliptical incision at the site of maximal fluctuation using a scalpel blade.
-
Drainage: Allowing the pus to drain freely.
-
Irrigation: Flushing the cavity with sterile saline to remove debris and bacteria.
-
Probing: Using a hemostat to break up loculations and ensure complete drainage.
-
Packing: Inserting sterile gauze (e.g., iodoform gauze) into the cavity to prevent premature closure and promote continued drainage .
3. Antibiotic Therapy
While I&D is often sufficient, antibiotics are indicated in certain cases:
-
Systemic Symptoms: Presence of fever or malaise.
-
Immunocompromised Patients: Individuals with conditions like diabetes or those on immunosuppressive therapy.
-
High-Risk Locations: Abscesses near vital structures (e.g., face, perianal area).
-
Recurrent Infections: Multiple abscesses or frequent recurrences.
-
Empiric Therapy: Common choices include clindamycin, trimethoprim-sulfamethoxazole, or doxycycline, especially to cover methicillin-resistant Staphylococcus aureus (MRSA) .
4. Post-Procedure Care
-
Wound Care: Keeping the wound clean and dry, and changing dressings as recommended.
-
Follow-Up: Scheduling a follow-up appointment within 24–48 hours to assess healing and remove packing if present.
-
Signs of Complications: Monitoring for signs of infection recurrence or complications such as cellulitis .
⚠️ Special Considerations
-
Location-Specific Abscesses: Certain areas require specialized care due to potential complications:
-
Perianal Abscesses: May lead to fistula formation and require surgical consultation.
-
Facial Abscesses: Proximity to vital structures necessitates careful management to avoid complications like septic phlebitis .
-
-
Immunocompromised Patients: These individuals may have atypical presentations and require more aggressive treatment and monitoring .
📚 References
-
StatPearls. Incision and Drainage.
-
Children’s Hospital of Philadelphia. Cellulitis/Abscess Clinical Pathway. CHOP Pathways
-
UCSF Hospital Handbook. Incision & Drainage. UCSF Hospital Handbook
-
Medscape. Abdominal Abscess Treatment & Management. Medscape
If you have further questions or need clarification on any aspect, feel free to ask!